What exactly is trauma? Simply, psychological trauma is a response to a stressful event. You might think of someone who survived 9/11, Hurricane Katrina, the California wildfires, or a combat veteran. These events are known as big “T” traumas.
Little “t” trauma are stressful events in which the individual coping skills are not enough. Some examples of little “t” traumas might be infidelity, divorce, abrupt or extended relocation, financial problems, or legal issues. Most tend to overlook these smaller events by rationalizing them as common everyday situations. Justifying them is a form of avoidance and can lead to feelings of shame.
What are the Symptoms of Trauma?
If left untreated, a person could experience mental health issues like addiction or post-traumatic stress disorder (PTSD).
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the criteria for PTSD includes being exposed directly or indirectly to a life-threatening, serious injury or sexual violence experience.
Other symptoms are classified as an intrusion, avoidance, and arousal. Intrusion can be experienced through memories, dreams, or flashbacks. Avoidance of memories and reminders are common symptoms with PTSD. Arousal symptoms include irritability, self-destructive behavior, hypervigilance, easily startled, difficulty concentrating, and sleep disturbance.
Long-Term Negative Effects of Trauma
Addiction
Substance use and PTSD have been strongly correlated. One study found that alcohol and drug consumption was associated with more significant PTSD symptoms 1 year after a disaster. Women who used drugs were more likely to exhibit signs of PTSD.
Early experiences of trauma also increase the risk of using drugs or alcohol to self-medicate. There is a correlation between childhood trauma and substance abuse, and they are not always from childhood abuse. For example, a child who moved or relocated because their parents divorced experienced a little “t” trauma. This experience may or may not result in substance abuse. However, childhood traumas remain and follow the person into adulthood, increasing the risk for self-medicating.
Eating Disorders
Approximately 30% of persons who were sexually abused in childhood had disordered eating. Bulimia nervosa and binge eating disorder were more likely to develop than anorexia nervosa among those with childhood sexual abuse histories. Although there is a correlation between trauma and eating disorders, it does not mean one causes the other.
One study found that traumatic events are positively associated with a negative self-image, psychosocial impairment, and conditions like anxiety and depression.
An internalized belief resulting from trauma is “I am unlovable.” If I am unlovable is believed, the individual may seek comfort in food. Food is not judgmental and allows the person to develop a pattern of avoiding emotions. The avoidance can lead to acting out behaviors too.
Romantic and Social Relationships
Early trauma events can impact trust. A breakdown in trust can lead to intimacy issues in our adult relationships. Trauma influences the way we attach to others. For instance, we might push others away or cling so tightly that they leave us. Our attachment styles can have a significant impact on our relationships.
How Does Trauma Affect the Brain?
Trauma and stress result in changes in brain regions like the amygdala, medial prefrontal cortex, and the hippocampus.
Amygdala
The amygdala is vital for safety and survival. This region of the brain alerts us to threats in our environment. If we are threatened, afterward, it might be challenging to concentrate or interact with others. The amygdala is responsible for the arousal symptoms of PTSD. Feeling jumpy or on edge is the amygdala alerting you to danger.
Medial Prefrontal Cortex
The medial prefrontal cortex helps mitigate the amygdala by reducing reactivity. This region is also responsible for decision making and for emotional responses. If the amygdala senses fear, the prefrontal cortex helps rationalize the fear.
Broca’s area is located within the prefrontal cortex and is responsible for language. Have you wondered why you struggle with verbalizing your trauma? The Broca’s area shuts down when confronted with trauma. The amygdala and the Broca’s area cannot compete with one another, making it difficult to put thoughts into words. Brain scans showed that when combat veterans triggered a flashback, their Broca’s area went offline. Merely shutting down can be a typical response to trauma.
Hippocampus
The hippocampus is responsible for learning and memory. Trauma likely affects how memories are stored and retrieved. For instance, you might remember some details, but not others. One study showed that shrinkage in the hippocampus might be related to ongoing dissociation and misinterpretation of threatening information.
What Treatments are Available for Trauma?
Cognitive Processing Therapy (CPT)
CPT is 12 weeks, with each session lasting 60 to 90 minutes. Therapy involves talking about the traumatic event and any related thoughts with your therapist. Next, you will write in detail, which helps process thoughts about the trauma and find new coping methods.
Prolonged Exposure Therapy
This treatment works well with avoidance symptoms and will help you learn to confront them. Prolonged exposure therapy is usually 15 sessions that are 90 minutes each. You will learn breathing techniques to alleviate anxious feelings about the trauma. You will also list various ways you have avoided the trauma and learn how to face them. Eventually, you will detail your trauma and listen to a recording of your account. This homework is thought to ease trauma symptoms.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR usually lasts 3 months consisting of 8 phases. Instead of talking about your trauma, you watch or listen to something your therapist is doing. It might be a light flashing or a moving hand that you will concentrate on. You will provide a history so that you and your therapist can identify distressing memories on which to focus. Your therapist will ensure that you have adequate coping skills to work through vivid imagery, negative beliefs about self, and the related emotions and body sensations. Near the end of EMDR, you and your therapist will examine your progress.
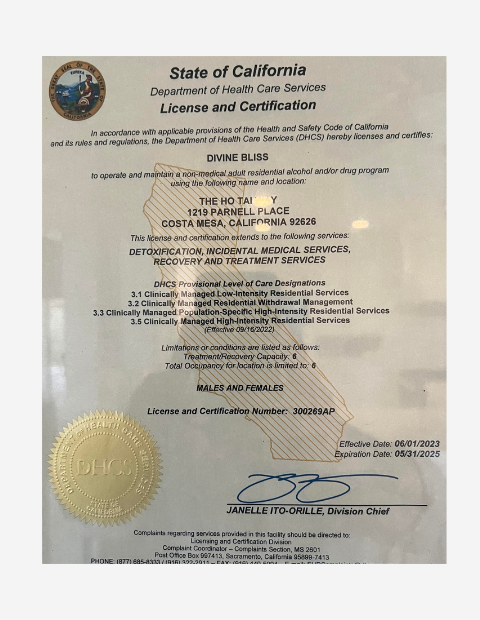
The Ho tai Way – Recovery for Women is here to help you work through your trauma and substance abuse issues. Please reach out to our admissions department if you are ready to heal. Call (714) 581-3974.