Does alcohol make depression worse? Alcohol can indeed exacerbate depression. It may provide temporary relief but ultimately deepens the depressive state through various physical and psychological impacts.
Depression and alcohol abuse often go hand in hand, creating a challenging cycle that affects many, especially women.
While some turn to alcohol to ease the symptoms of depression, it can counterintuitively worsen their mental health. Understanding the relationship between these two issues is vital for effective treatment and recovery.
In this article, we will explore the following:
- Does alcohol make depression worse?
- How alcohol use makes depression worse
- Breaking the cycle of co-occurring depression and alcoholism
- How alcohol rehab for women can help
Does Alcohol Make Depression Worse?
Alcohol’s effects on depression are far-reaching and detrimental. It alters brain chemistry, affecting mood and emotional regulation.
This impact is particularly pronounced in women, who may experience more severe consequences due to biological and hormonal differences.
Research shows alcohol misuse among women is increasing. Women who drink have a higher risk of certain alcohol-related problems compared to men.
Here are several ways alcohol makes depression worse.
Mood Swings
Alcohol’s impact on mood swings is particularly significant for women dealing with depression. Initially, alcohol may seem to offer a reprieve from the heavy feelings of sadness or hopelessness, but this relief is fleeting.
As a depressant, alcohol can actually lower mood levels, leading to an intensified state of depression once the initial effects wear off.
Over time, regular alcohol consumption can disrupt the brain’s chemical balance, leading to more frequent and severe mood fluctuations. These mood swings are not just limited to feelings of sadness but can also include bouts of irritability and anger. This volatility in emotions makes it increasingly difficult for individuals to manage their depressive symptoms, maintain relationships, and handle daily responsibilities.
The inconsistency in mood further complicates the process of finding a stable, effective treatment for depression, as the ups and downs caused by alcohol make it challenging to assess the true baseline of one’s emotional state.
Sleep Disturbances
Sleep disturbances caused by alcohol are a significant concern for women with depression. While alcohol might initially seem to help with falling asleep, its overall impact on sleep quality is negative.
Alcohol disrupts the sleep cycle, particularly affecting the REM (Rapid Eye Movement) stage, which is crucial for a restful and restorative night’s sleep. This disruption often leads to a lighter, more fragmented sleep, causing individuals to wake up feeling tired and unrefreshed. Poor sleep quality exacerbates depressive symptoms, such as low energy, difficulty concentrating, and a general sense of malaise.
For women, the interaction between disrupted sleep and hormonal fluctuations can further complicate the situation. Sleep deprivation can lead to heightened emotional reactivity and sensitivity, making it more challenging to manage stress and maintain emotional stability.
The ongoing cycle of poor sleep and intensified depression creates a detrimental feedback loop, hindering both mental and physical well-being.
Increased Anxiety
Increased anxiety is a common yet often overlooked consequence of alcohol use in women with depression.
Initially, alcohol may be used as a self-medication tool to alleviate feelings of anxiety. However, as the effects of alcohol wear off, anxiety levels often rebound to higher levels than before.
This is due to alcohol’s impact on neurotransmitters in the brain, such as serotonin and GABA, which play key roles in regulating mood and anxiety. When these neurotransmitters are disrupted, it can lead to increased feelings of anxiety, panic, and stress.
For women, these effects can be more pronounced due to differences in body composition and hormone levels, which may affect how alcohol is metabolized and its impact on the brain. The increase in anxiety can worsen depressive symptoms, creating a cycle where alcohol is continually used to mitigate anxiety, only to lead to greater levels of anxiety and depression over time.
This pattern can be particularly debilitating, as it impairs the ability to manage daily tasks and maintain social connections, further isolating the individual.
Dependence Risk
The risk of developing a dependence on alcohol is a significant concern for women using alcohol to cope with depression.
This dependence can develop as the body and mind begin to rely on alcohol for emotional relief or to escape depressive symptoms.
Over time, tolerance to alcohol increases, meaning larger amounts are needed to achieve the same effects, leading to more frequent and heavier consumption. Biological factors, such as differences in how women metabolize alcohol, can accelerate the development of dependence.
This dependence complicates the treatment of depression, as it introduces a dual diagnosis of substance use disorder alongside depression. Withdrawal symptoms from alcohol can mimic or exacerbate depressive symptoms, making it challenging to distinguish between the two conditions.
The cycle of dependence also impacts self-esteem and personal relationships, further entrenching feelings of hopelessness and helplessness associated with depression.
Breaking this cycle requires comprehensive treatment that addresses both the substance use disorder and the underlying depression, acknowledging the complex interplay between the two.
Reduced Effectiveness of Medications
The interaction between alcohol and medications prescribed for depression is a critical concern.
Alcohol can significantly reduce the effectiveness of antidepressants and other mental health medications. This occurs due to alcohol’s impact on the body’s ability to metabolize and absorb these medications, as well as its direct interference with the brain’s neurotransmitters.
Women, in particular, may experience more pronounced effects due to differences in body composition and metabolism, which can alter how drugs and alcohol are processed. Additionally, alcohol’s depressant effects can counteract the benefits of antidepressants, leading to a lessened therapeutic effect.
This reduction in medication effectiveness not only hinders the treatment of depression but can also lead to a false perception that medications are ineffective, potentially causing individuals to discontinue their prescribed treatment.
The combination of alcohol and medications can also lead to unwanted side effects, further complicating the management of depression and overall health.
Impaired Judgement and Decision Making
Alcohol consumption can significantly impair judgment and decision-making abilities, particularly in individuals struggling with depression.
When under the influence of alcohol, the brain’s frontal lobe, responsible for decision-making and rational thought, becomes less active. This leads to impaired judgment and a tendency to make poor or risky decisions that one might not make when sober.
For women, these impaired decisions can have far-reaching consequences, including engaging in unsafe behaviors or neglecting responsibilities. The regret and guilt that often follow such decisions can worsen depressive symptoms, creating a cycle of drinking, poor decision-making, and deepening depression. Additionally, impaired judgment can strain personal and professional relationships, further isolating the individual and exacerbating feelings of loneliness and despair.
This cycle highlights the importance of addressing both alcohol use and depression in a comprehensive treatment plan.
Physical Health Problems
Chronic alcohol use can lead to a multitude of physical health problems that exacerbate depression.
These issues include liver disease, cardiovascular problems, and neurological damage, among others. For women, the health consequences can be more severe due to biological differences in how their bodies process alcohol. These health issues can create a significant psychological burden, adding to the stress and anxiety that accompany depression.
The physical discomfort and limitations caused by these health problems can further hinder an individual’s ability to engage in activities they enjoy or fulfill daily responsibilities, leading to feelings of helplessness and lowered self-esteem.
The awareness of deteriorating physical health can also deepen depressive symptoms, creating a feedback loop where physical health issues worsen depression, which in turn leads to more alcohol consumption as a form of self-medication.
Social and Relationship Issues
Alcohol use can have a profound impact on social interactions and relationships, areas that are already often strained in individuals with depression. Alcohol may initially seem like a social lubricant, but its abuse can lead to behaviors that strain relationships, such as aggression, withdrawal, or emotional volatility.
Women might find that their relationships with family, friends, and colleagues suffer as a result of their alcohol use, leading to social isolation and a lack of support networks that are crucial for managing depression. This isolation can intensify feelings of loneliness and worthlessness, key aspects of depression. Additionally, the stigma associated with alcohol abuse can make women reluctant to seek help, further isolating them.
The impact on relationships is not just emotional but can also be practical, as it may affect one’s ability to maintain employment or fulfill family responsibilities, adding additional stress and exacerbating depressive symptoms.
Negative Coping Strategy
Using alcohol as a coping mechanism for depression is a negative strategy that can have far-reaching consequences.
Initially, alcohol might seem to offer temporary relief from depressive symptoms, but this is a deceptive and short-lived solution.
The primary issue with this coping strategy is that it avoids addressing the root causes of depression. Instead of dealing with the underlying emotional pain, challenges, or trauma, alcohol use only masks these issues, delaying necessary psychological processing and healing.
For women, this reliance on alcohol can lead to a worsening of depressive symptoms in the long term. Furthermore, using alcohol as a coping tool can also lead to the development of unhealthy habits and behaviors, reinforcing the cycle of depression and alcohol abuse.
It’s a coping mechanism that not only fails to solve the problem but often exacerbates it, creating additional layers of psychological and emotional complexity that need to be addressed for effective recovery.
Emotional Numbing
Alcohol’s ability to numb emotions is often why individuals with depression may turn to it, but this numbing effect is detrimental to mental health.
Emotional numbing means that while alcohol can temporarily dull feelings of sadness, anxiety, or distress, it also impairs the ability to experience positive emotions like joy, contentment, and hope.
This emotional blunting can leave individuals feeling disconnected from their own experiences and those around them. For women, emotional numbing can interfere with personal relationships, parenting, and professional responsibilities, as it hinders the ability to engage fully and authentically in various aspects of life. Additionally, the numbing effect of alcohol prevents individuals from processing and working through the emotions and experiences at the root of their depression.
This avoidance can delay recovery and healing, as it is through confronting and managing these emotions that individuals can move forward in their mental health journey.
Breaking the Cycle of Co-occurring Depression and Alcoholism
Breaking the cycle of co-occurring depression and alcoholism is a challenging yet achievable journey that requires a multifaceted approach.
Central to this process is the recognition that both conditions are deeply intertwined, each often exacerbating the other.
Effective treatment must address both the depression and the alcohol dependency, with an emphasis on holistic care. This includes cognitive behavioral therapy sessions that help to reshape thought patterns and behaviors, coupled with medical treatment such as antidepressants, if necessary.
Support groups and a strong network of understanding friends and family members can provide crucial emotional support. Additionally, developing new, positive coping strategies is vital. This might involve activities such as mindfulness practices, physical exercise, or engaging in fulfilling hobbies.
Lifestyle changes, including improved diet and sleep habits, also play a significant role. Patience and self-compassion are key, as recovery is a gradual process with potential setbacks.
With commitment and the right support from friends, family, and a women’s addiction treatment center, individuals can successfully navigate this path, leading to a healthier, more balanced life.
Need Help Overcoming the Cycle?
Are you or a loved one struggling with the intertwined challenges of depression and alcoholism?
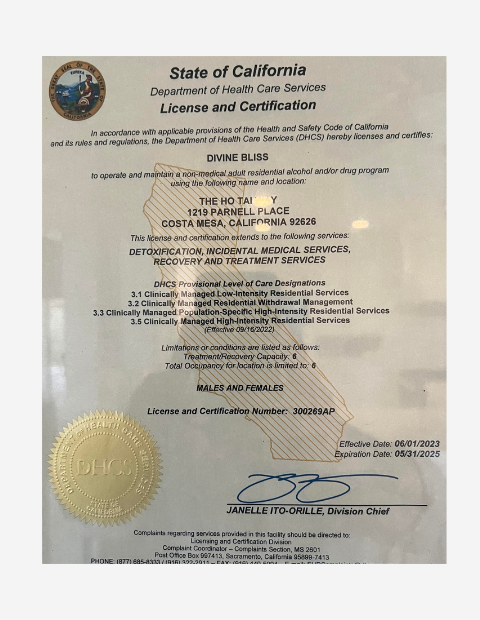
At The Ho Tai Way, we understand the unique struggles women face in this journey. Our compassionate, personalized treatment programs are designed to support you in breaking free from this cycle and embracing a healthier, more fulfilling life. Start your path to recovery with us, where hope and healing meet.
Contact us today to learn more about our alcohol rehab for women in Costa Mesa, California.
Conclusion
Alcohol indeed makes depression worse, especially for women attempting to self-medicate. Understanding this relationship is crucial in addressing both depression and alcohol abuse effectively.
With the right support and treatment, it is possible to break this cycle and move towards a healthier, more positive future.